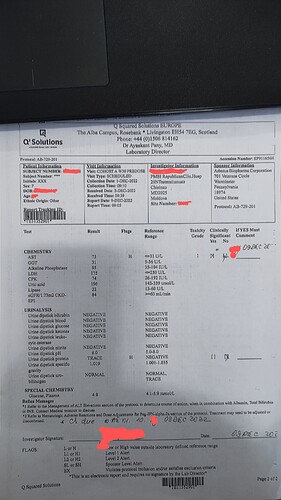
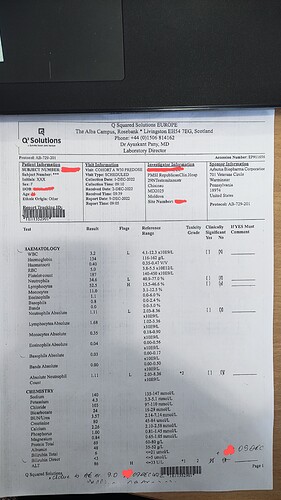
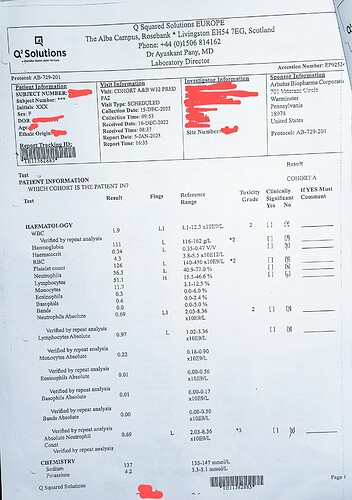
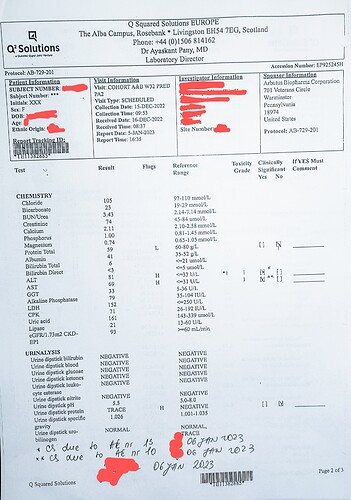
My WBC, and neutrophils are below the reference range but ALT, AST, Lymphocytes and urine protein are higher than reference range. I go twice a month to the clinic and the other two injections I asked a nurse from our local clinic to help me with the injection, I can’t do it on myself  .
.
I was told on week 24 the arm I was randomised (A1, 24 weeks of Interferon plus two more AB-729).
I am glad you are doing fine with AB-729 and hopefully will be the same with Interferon 
Thank you for the information since you are a little ahead of me! I wish you a continued easy time symptom wise and hope for hbsag loss for you! Keep in touch and I’ll do the same!
Indeed tolerability for pegIFN is very different (better) for patients with HBV infection than patients with HCV infection. This is for two reasons: 1) pegIFN is given with ribavirin in the treatment of HCV which causes additonal adverse reactions and 2) HCV is a viral infection which responds differently to pegIFN than HBV infection. These issues have been well defined in large clinical studies. The confusion amongst patients and doctors alike regarding these issues is unfortunate.
With treatment of HBV infection, pegIFN therapy is accompaned by mild flu like symptoms and mild reductions in platelets and white blood cells which normally have no impact on your health. Very rarely a patient might experience stronger declines in platelets which can be easily managed with supportive medication. Your doctor will know how to help you. I would not be so worried.
Not being able to see your antiviral response is an unfortunate complication of the way in which many trials are designed. However, seeing a strong elevation in liver enzymes (ALT and AST) predicts HBsAg loss and functional cure during pegIFN therapy. You can keep an eye out for these events in your blood work.
Good luck!
Very good information, thank you! My WBC (neutrophils only - but this seems to make up most of wbc) is naturally on the very low end of normal, rarely has been below normal range. This is something that I’m told is my “normal” since I’m otherwise a healthy person/normal reacting immune system. However, knowing this is a concern of mine with interferon. My platelets are always in the complete normal range, so no concerns there ever.
Thanks again for your expertise and help!
Hi availant,
I always appreciate your effort, and huge experience guiding every of us here.
Please, would you advise me to join this? And if your response is yes, how can i go about it ? As i currently stay here in Hobart, Australia.
Thanks
Evans
Thank you for the valuable information you give us!
In your opinion, how much is a strong elevation in liver enzymes?
Thanks!
Looking forward to hearing from you how you’re doing with Interferon 
Lord’s blessings!
Dear @Evans,
In general, RNAi in HBV have been shown to be safe and well tolerated with the exception of injection site reactions. A similar combination trial with NUCs, RNAi (VIR-2218) and pegIFN has recently shown HBsAg loss in 30% of subjects at the end of therapy but many patients in this trial had low baseline HBsAg (as low as 50 IU/mL) and there was no control group with NUCs + pegIFN in this study to assess the impact that RNAi actually had. No follow-up data is available yet to see of any of the HBsAg loss translates into functional cure.
Based on this data, there is no reason for you to not consider enrolling in this program.
The sites enrolling for this trial can be found here. There are two sites still recruiting in Australia.
You can consult with your physician regarding this.
Best regards,
Hi @Ecky
An ALT elevation > 3x the upper normal limit (ULN) is considered a flare. Strong flares are typically 5-10x ULN or more.
Best regards,
Thanks for your replay!
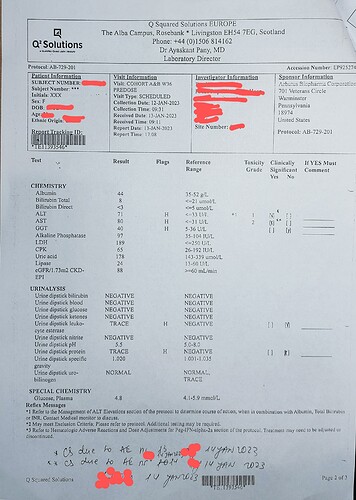
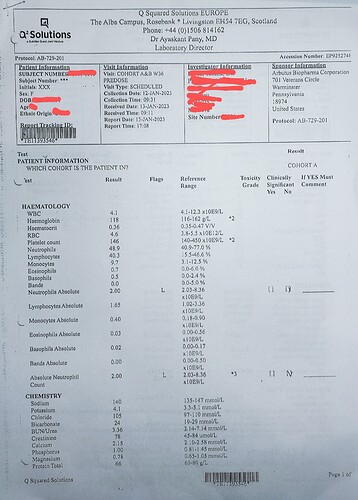
I attach here my blood work results from last month (haven’t received yet the most recent results), could this be a sign of HBsAg loss or it’s too early and not strong elevation to predict it?
Hi @Ecky
Your liver metabolic function (bilrubin and albumin) are normal and platelets are also ok. This means that the very mild ALT elevation you are seeing is likely immune mediated (which is a good thing). Flares of this magnitude are very common in patients receiving pegIFN who do not achieve HBsAg loss and functional cure.
It is important to realize that this single time point measurement could be the start, middle or end of a ALT flare. You have to watch these results over time. Also, depending on how frequently you are having these blood tests, you might miss some of the ALT flare.
Hope this helps.
I really appreciate all the valuable information you give us!
Hi 3kids4me,
Does it in any way cause any problem with those with genotype A? Just asking as you wrote it here
I’m not sure what you are asking regarding genotype A, please be more specific.
Thanks somuch for the response. My next appointment is on the 23rd and i hope to discuss it with the GI.
Thanks
@3kids4me
How are you doing?
Have you started yet Interferon?
I am nearly half way through it and started to experience some of the side effects like fast or irregular heartbeat, weakness in my legs and arms, persistent cough, dry mouth. Regardless of these I am able to work full time (I do need to rest after I climbed one or two floors ![]() ) and do my daily routine.
) and do my daily routine.
Also, the very mild ALT elevation persists.
Some of the experts, could you help me with an answer please, why GGT is above the normal range, is this usual to happen?
The blood work from 15 of December
The results from 12 of January
Thanks ![]()
I @Ecky,
I assume that you are taking NUC + ABI-729 + pegIFN?
Your ALT, AST and GGT elevations are only very mild and not really very concerning and very common during pegIFN therapy. These are not really elevated enough to be considered a liver enzyme “flare”.
Increased upper respiratory tract inflammation and hypersensitivity to seasonal infection have been reported for other siRNAs in development for HBV and for other indications and are likely driven by the off target stimulation of TLR3 by these agents. Hopefully you will have informed your physician about your persistent cough.
Mild fatigue is very common with pegIFN.
Fast or irregular heartbeat (especially if occurring while you are at rest) is extremely rare with pegIFN and may indicate cardiotoxicity. I am not aware of cardiotoxicity reported for siRNA. These symptoms should be reported to your doctor and taken seriously. If mediated by pegIFN, they usually resolve after removal of pegIFN.
Best regards,
Thank you for your answer!
Indeed, I am taking NUC + ABI-729 + pegIFN. Regarding fast or irregular heartbeat, it is not every day, but last night was the worst, I couldn’t sleep because of the tachycardia and headache. Thankfully I could sleep a few hours before I had to go to work ![]()
Hi Ecky,
I’m just a little behind you, I am scheduled to start IFN in about 6 weeks, with my week 20 appointment being on 2/6 and then a month after will find out which arm I’m in and start IFN. I’m glad you are hanging in there and letting me know some of your symptoms, so we can hopefully help each other though it soon. I’m getting nervous about the IFN, especially because I got COVID again last month and still have some lingering symptoms (that I’ve had in the past after a virus) I feel as a result of that. I’m going to ask at my next appointment, but if things don’t get under control with the other condition I don’t know if I’m going to be able/or want to add something else onto my system which I already am nervous about. Luckily, I haven’t had any issues with the AB729, but know the IFN is an important key to try and kick the HBV. I wish you continued luck and please continue to keep us posted!
I strongly advise you to consult your physician.
Tachycardia while resting should be taken seriously.