Hello everyone,
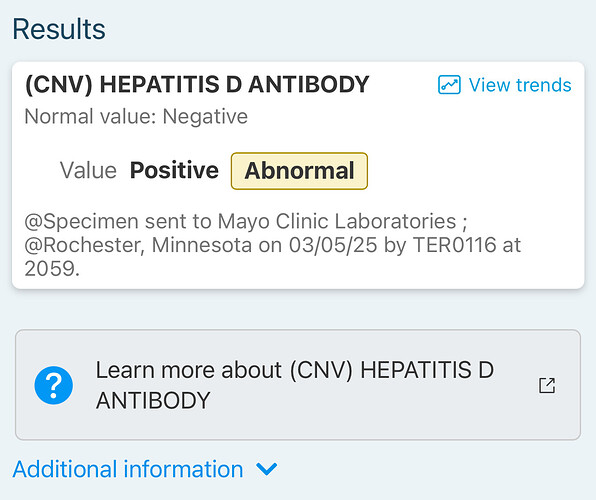
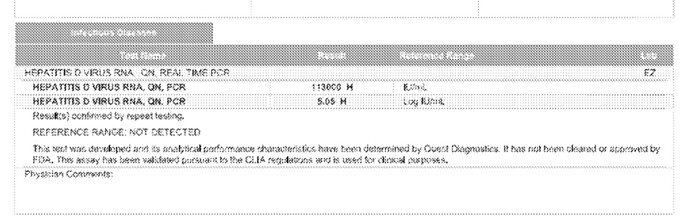
Just wanted to share an update and get some advice. I was recently diagnosed with Hepatitis Delta (HDV). Last month, my HDV antibody test came back positive, and a PCR test done by Quest Diagnostics here in the U.S. confirmed a very high viral load. I’ve attached the results for reference.
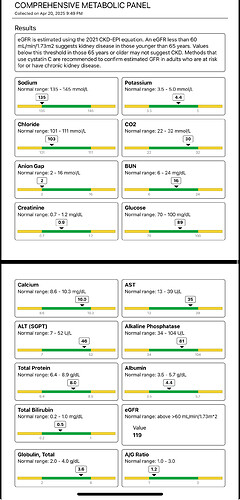
Before those results came in, my provider started me on Tenofovir (TDF) on March 15th due to elevated ALT and AST levels.
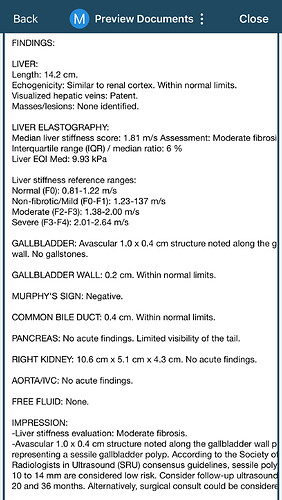
My most recent labs show that ALT and AST are beginning to normalize. My doctor’s current approach is to continue monitoring my liver enzymes and stay on TDF for now. He explained that PEG-IFN is the only FDA-approved treatment for HDV in the U.S., but its side effects can be quite harsh — comparable to chemotherapy. He said we’d only consider it if my enzyme levels or other markers worsen. Since he’s a general gastroenterologist, he also plans to consult with a hepatologist regarding the next steps.
I’m not sure if this is the best strategy, and I’d really appreciate any insights or shared experiences from others who’ve been through similar situations.
Separately, about a month after starting TDF, I developed persistent foamy urine and generalized edema. I went to the ER, and while all kidney markers came back normal and there was no protein in the urine, no specific cause was identified. I was told it could be due to recent weight loss, but I’m not convinced. The symptoms — foamy urine and puffiness — seem more consistent with kidney issues, which is concerning given I’m on TDF.
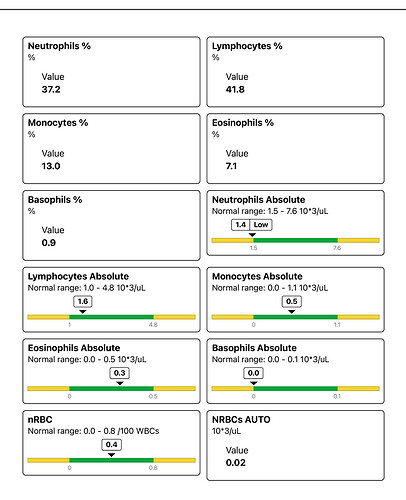
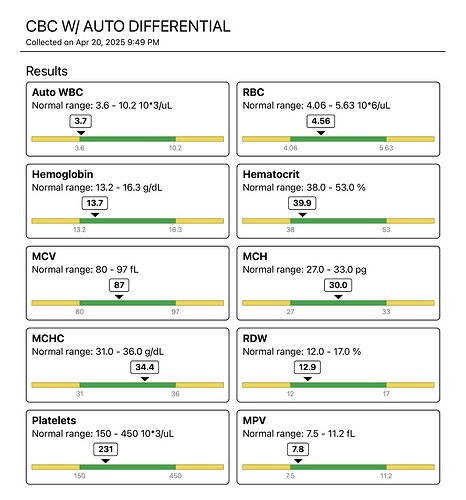
All my other labs were normal, except for a low white blood cell count.
I’d love to hear from anyone who has dealt with HDV treatment in the U.S. or abroad, especially in terms of:
• Best treatment options and outcomes
• Managing or identifying causes of edema while on TDF
• Whether my doctor’s approach sounds reasonable based on your experience
I really want to stay on top of this before it progresses. Thanks in advance for your help and support.
Here my previous post here:
https://www.hepbcommunity.org/t/my-hbv-lab-and-liver-elastography-results/7043/12?u=mmal_jr