My turn. ![]()
All bloods good. I am concerned about ultrasound though.
Mild coarsened echotexture of liver . No focal lesions . All surrounding organs good.
I’ve shortened the report.
Previously fatty liver. On Entecavir treatment last 5 years. Diet good, weight good, more exercise needed.
My liver seems to be going how I’ve said it would but professionals say nothing……except it’s not cirrhosis or liver cancer.
Am seen by my GP as specialists are 458km away. And seeing a GP is the way government has recommended.
Why is my liver progressing towards cirrhosis when I’m on treatment and look after my liver?
@ThomasTu @HealthExperts @availlant @john.tavis
Hi @Caraline ,
What is your latest HBV DNA and ALT?
Ultrasound is only a snapshot in time of your liver (this one appears to suggest only mild fibrosis) - do you have historical imaging to compare it to?
Progression of liver disease with successful response to NUC therapy is rare (this does not include liver cancer).
Hi @Caraline,
Agree with @availlant here. A better indicator of progression to cirrhosis may be a fibroscan that can distinguish between fatty liver (CAP score) and fibrosis level (kPa level)
Thomas
My alt is under the threshold from memory 22-25. HBV viral load is undetectable has been for years.
My Hepa score is 0.51
We don’t have a fibro scan in our town.
Thanks for replying
@ThomasTu @availlant
Dear @Caraline,
So with these HBV DNA / ALT numbers, I suspect the ultrasound findings could reflect one of the following:
-
Incomplete (and perhaps ongoing) recovery from more advanced fibrosis pre-treatment. Reversal of fibrosis is a very slow process following successful suppression of HBV replication.
-
Mildly fatty liver. Although if this is the case, inflammation is minimal as your ALT is normal. This is the case for many individuals with mild fat accumulation in their liver.
Dear @Caraline,
First, let me express my support for you as you work through these complex and scary issues.
I’m not a clinician and cannot give detailed diagnosis or prognosis. However, the liver is a really complex organ, and many factors can influence its health other than HBV. A few such factors include (not that I am NOT suggesting these are acting in your case, just listing possibilities): Fatty liver disease, chronic alcohol consumption, genetic propensity, autoimmune hepatitis, chronic HCV infection, dietary toxins such as aflatoxin that are endemic in some areas, chronic high-level acetominophen (ie, Tylenol) use, and chronic use of some prescription drug combinations (although this should be filtered out by your medical team). Some of these factors can work together to make things that are normally OK by themselves lead to disease progression (for example, chronic HCV infection increases sensitivity to alcohol-mediated liver damage). Discussing some of these possibilities with your physician might help.
I wish you the very best,
John
Thank you @john.tavis . I really appreciate your response and care.
I don’t drink, smoke, and very careful with my diet and chemicals.
I am on quite a few medications but my doctor says I need them.
Five years ago there was nothing wrong, unremarkable, with my liver.
Then it went to fatty liver and now Mild coarsened echotexture of liver.
I don’t eat fried food, chips, biscuits, junk food, flavoured soft drinks, added sugar or sugar substitutes. Drink lots of black coffee, cook my own food, make my own yoghurt. I do indulge in cake or sweets on weekends. I don’t have HCV. Btw I’m 63. My stomach is protruding. I look like I’m pregnant but ultrasound didn’t say I had any inflammation in the surrounding organs. I weigh 57kg 160cm and shrinking ![]()
I don’t know if I’m being paranoid or it’s old age or something isn’t right. ![]()
I think I’m doing everything right so why isn’t my liver?
Thanks for your understanding.
Dear @Caraline,
You live a healthier life than I do (and we’re about the same age)!
Your question is beyond my expertise (I’m a molecular virologist specializing in HBV replication mechanisms). I recommend speaking with a hepatologist who specializes in viral hepatitis, and getting a second opinion if the answer you get is unclear. Until then, continuing regular screening is very likely merited.
I wish you the best.
John.
Hi @Caraline,
I read about your concern regarding a recent ultrasound. I understand your frustration, stemming from the fact that you have been doing everything to protect your liver and stay healthy but results from tests sometimes goes the other way. You are not alone here. About 9 years on treatment here and I have similar problem. Some patients seem to deal with this problem while others don’t. The good thing here is that it is not cirrhosis or liver cancer. I understand that fatty liver can sometimes complicate hepatitis B treatment at least that is what my provider thinks in my case. We just have to keep doing what we know how to do and let the results fall where they will fall. I understand how concerning this can be but we cannot control some of these test results. Don’t let this keep you down, keep up with the good work you have been doing. Take it one day at a time. Cheers, Bansah1.
Dear @Caraline ,
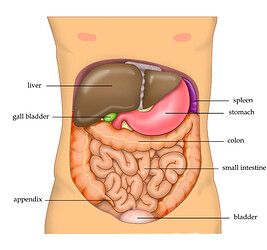
As John mentioned, following up with your physician is important. This is especially true given your description of a “protuding stomach” with a normal body mass index (based on your height and weight this is 22.3 which is in the normal range for adult women). This protrusion in your abdomen may not actually be your stomach but your liver as sometimes the presentation of liver issues is not obvious to the layperson (the liver actually sits on top of your stomach).
Again your most recent ALT is normal so this is at odds with severe fatty liver. You may also want to consult a dietitian. It may be that you also need to think about removing foods with a high glycemic index from your diet. These foods contain starches which are easily broken down by the body and lead to fat accumulation similar to the other foods you have already excluded from your diet. High glycemic foods include potatoes, parboiled rice, any baked goods prepared with enriched white flower, and well cooked pasta and root vegetables (like carrots).
Thank you for your advice. I really appreciate it and the picture helps too.
Thank you @Bansah1.
My rebellious side wants to go and undo all my hard work. It’s like…what’s the point. I might as well go out eat, drink smoke and me merry😂
But I won’t.
KFC for breakfast lunch and dinner ![]()
Take one day at a time.
I’m noticing a pattern here.
Every six months, after test results, I get depressed and anxious for about a month!
Then I move on. Say, whatever will be , will be.
It’s hard not being able to tell my friends too. For me, I will never be able to tell them. It’s like telling them I have an STI. I sometimes think it will be easier if I have cancer and I could tell people. But I do not wish that.
Thank you everyone for pitching in. I appreciate it all.
Hi @ Caraline,
I hear you and I do empathize with you.
While I understand the notion that we take one pill a day and all will be fine, but that is not always true. Some people with this disease deal with anxiety, depression, among other mental and psychological issues. Don’t even mention the physical ordeal some patients go through. It’s a lot to deal with. Whenever I tell people about my condition I see them looking at me like I am stupid or something. They don’t believe me because to them I look good on the outside. It’s difficult to explain/share what we deal with.
We all have to do the best we can and take things one day at a time. Lets continue to remain hopeful for a cure whenever that happens. We cannot give up now, we have come too far to relent. I know it’s not easy to continue to hold on. But we all have to try.
Take a deep breath, tomorrow might be a better day. I send some strength your way.
Best, Bansah1.
4 posts were merged into an existing topic: Lifestyle changes, nutrition, and supplements for hep b
Aww thank you @gregory your words have encouraged me greatly.
To be understood is healing.
Hi John,
Just curious about hep B virus. I understand that the cccDNA exist inside the hepatocytes . Recently, I learn that they are also found in the telomere. I am not sure how the virus find their way to telomere. And any of those two could cause HCC? Which will be more likely that cause HCC
Thanks very much
Carlos
Dear @Ccheng8346,
The cccDNA does indeed exist in the nucleus. It remains as an “episome”, or small circle that is not integrated into the cell’s DNA. This contrasts it from integrated DNA that accumulates in HBV+ cells, where the HBV DNA is inserted into the cell’s DNA, literally becoming part of the cell’s chromosomal DNA (ie, “covalently linked” into the cell DNA). Integration happens during a failure to convert the relaxed circular DNA found in viruses into cccDNA. The HBV DNA is vastly smaller than the cell’s DNA, and it inserts into the cell DNA more or less randomly. Sometimes by pure chance it inserts near one of the chromosome ends (the “telomeres”).
The cccDNA itself does not directly induce cancer, although it certainly contributes to it by being the DNA that makes the viral proteins (some of which have tumor-promoting abilities, especially HBx). HBV proteins also trigger the inflammatory environment in the liver as the immune system tries to get rid of HBV. It is the long-term inflammation in the liver that is believed to be the major (but not only) way HBV causes cancer.
The integrated DNA can have direct oncogenic effects in 2 ways. First, if it somehow inactivates a “tumor suppressor” (ie, a gene that prevents cells from dividing when they are not supposed to), for example by integrating into the gene and destroying it, then the “brakes” on cell division are weakened. Second, if the HBV DNA integrates in a way that turns on a “proto-oncogene” (ie, normal cell proteins that promote cell division when then cell needs to do it), for example by placing one of the viral enhancers near enough to turn up production of the proto-oncogene, it can push the cell towards cell division when it is not supposed to do so. HBV integration near the telomeres can affect cell cycle regulation, but I cannot remember off-hand what the mechanism is.
I hope this helps.
John
Dear John,
Thank you so much for the wealth of information you provided . I appreciate it immensely, to make matter short . I have hep B with genotype C which is more virulent than genotype B. I had cirrhosis of the liver 15 yrs ago and where able to overcome it. Fibroscan shows stage 1 and my ALT is in the 15-16. AFP are always normal<3, and all tumor markers are normal. Suddenly , my ultrasound shows a 4.6 cm lesion . I was advised to get liver resection last year . Things looks fully recovered. I was talking to my hepatologist and just like what you described, he believed the HVB DNA insert itself into telomere . Not sure they found the telomere to contain the hvb DNA in the biopsy. I know there is a chance it could come back . But he believe it will be remote at this time ( he told me some of his patient has resection 15 yrs ago and going strong . I also read about to MAb that they used to prevent reoccurrence of HCC. I am hopping they can find a functional cure soon.
Thank you so much again . I remain grateful for your information
With deep appreciation,
Carlos
Hello Carlos @Ccheng8346
That’s fantastic you were able to overcome cirrhosis and your fibroscan is so low.
Well done.
I hope all goes well with your liver resection and MAb treatment.
We are here for you, Carlos.
Unfortunately , after 15 yrs I came down with HCC last June 2023. Had liver resection and Just got blood work normal.